We Need Full Approval Of COVID-19 Vaccines, But Only After Careful Evaluation
It’s been about six months since the Food and Drug Administration allowed the distribution of the first COVID-19 vaccines via emergency use authorizations, which are preliminary approvals during a public health emergency based on lower standards of safety and efficacy than for a normal, or “full,” approval. As of July 13, 48.1% of the U.S. population had been fully vaccinated.
However, uptake has been inconsistent among different groups and locales, the earlier momentum for vaccination has waned, and there are surges of infections in various under-vaccinated parts of the country. There are many reasons for that, including skepticism about COVID-19 as a threat, worry about the vaccines’ safety, and concern that the vaccines are “experimental” because they continue to be marketed under EUAs’ lower standards. A recent Kaiser Family Foundation survey found that about one-third of adults who have not yet been vaccinated would be more likely to get a vaccine that is fully approved by the FDA, which Pfizer applied for in early May, and Moderna applied for on June 1.
To relieve the concern about getting vaccines that haven’t received full approval, a number of prominent physicians and public health experts have called for the FDA to grant approval immediately. Dr. Megan Ranney, an emergency room physician and professor at Brown University, said, “I wish the FDA would move faster,” and added, “Full FDA approval process normally [takes] months, but they’ve already looked at the preliminary data. It’s not that much more.”
Dr. Eric Topol, a professor of molecular medicine at Scripps Research who has served on FDA advisory panels, noted in a July 1 op-ed that the EUAs “were granted after the agency reviewed the results of clinical trials that involved more than 70,000 participants [and] … now more than 180 million doses of the Pfizer vaccine and 133 million of Moderna’s have been administered in the United States, with millions more doses distributed worldwide. In the history of medicine, few if any biologics (vaccines, antibodies, molecules) have had their safety and efficacy scrutinized to this degree.” He concluded that there has been “more than ample time for the agency to conduct plant inspections and review the applications,” and that “the stakes could not be higher.”
I am sympathetic to those arguments, but the reality is that the stakes are higher. The history of drug and vaccine development illustrates the possible pitfalls, some of which have had dire effects. The most notorious was the catastrophic “Cutter Incident,” in which, in 1955, more than 200,000 children in five Western and Midwestern states received a polio vaccine in which the process of inactivating the live virus proved to be defective. Within days, there were reports of paralysis, and within a month, the first mass vaccination program against polio had to be abandoned. Subsequent investigations revealed that the vaccine, manufactured by the California-based family firm of Cutter Laboratories, had caused 40,000 cases of polio, leaving 200 children with varying degrees of paralysis and killing 10.
The Pfizer-BioNTech and Moderna vaccines are not killed-virus vaccines, so faulty inactivation is not a possibility, but drug and vaccine manufacture are highly complex. Earlier this year, for example, the FDA recalled certain batches of a commonly prescribed diabetes drug, metformin, because it contained unacceptably high levels of a cancer-causing chemical contaminant.
Nor has the production of COVID-19 vaccines escaped serious problems. Emergent Biosolutions, which was designated by the U.S. government to be the sole domestic manufacturer of the vaccines developed by Johnson & Johnson and AstraZeneca, has had to discard 75 million vaccine doses because of possible contamination. Production at Emergent’s Baltimore factory has been halted for more than two months as the company tries to convince regulators that it has remedied safety problems FDA inspectors identified earlier this year.
There are several critical points here. First, although the major pharmaceutical companies are generally extremely experienced and proficient, sometimes, as is the case for at least some of the COVID-19 vaccines, they contract with other manufacturers that might be less fastidious and that need careful regulatory scrutiny to ensure safety and efficacy.
Second, the medical and public health experts who are, with the best of intentions, demanding the immediate full approval of the COVID-19 vaccines, have not actually reviewed the critical data (which run to hundreds of thousands of pages). When I was an FDA medical reviewer evaluating the first genetically engineered drugs and vaccines in the 1980s, my office looked much like this, except that each application was several times larger:
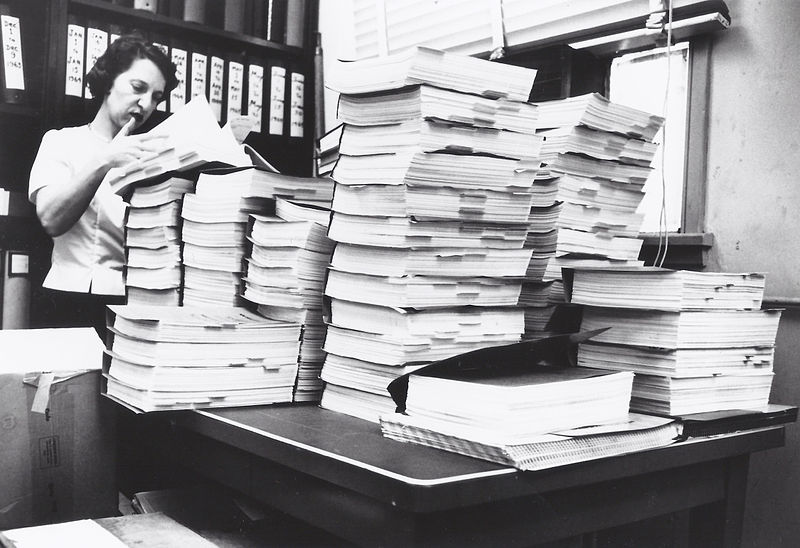
Courtesy: U.S. Food & Drug Administration
Applications are extraordinarily complex and sometimes contain shortcomings or inconsistencies, and the inspections of manufacturing facilities may raise concerns.
There is also the “big picture” issue: If the FDA were to grant full approval to a product that caused a debacle similar to the Cutter Incident, or even a problem like the recent metformin contamination, it would not only injure patients but also provide fodder for anti-vaccine activists and make the public skeptical of vaccines in general for years, or even decades. Those are the really high stakes.
We do need full approval of the COVID-19 vaccines and as quickly as possible, but it should be granted only after the manufacturers demonstrate the ability to produce batch after batch with the necessary purity, potency, and sterility.
Henry Miller, a physician and molecular biologist, was a research associate at the National Institutes of Health and the founding director of the FDA’s Office of Biotechnology.
Read More
